By Dr. Aylah Clark
Inflammation comes up a lot in my practice. It promotes many chronic diseases and correlates with worsening signs and symptoms of many conditions, whether it be autoimmune disease, arthritis, cardiovascular disease, or others. Inflammation is also intrinsically tied to obesity. How are inflammation and body weight related and what can we do about it?
What is inflammation?
Inflammation is your body’s attempt to protect itself. It involves complex biological processes that are activated by things like foreign invaders (bacteria and viruses for example) or damaged cells (injury). We need inflammation to protect ourselves from these harmful events and to initiate healing, but we want this inflammation to finish its job. When it doesn’t, or there is always a stimulus promoting inflammation, we get chronic inflammation. Chronic inflammation is associated with chronic diseases like autoimmune disease, atherosclerosis, cancer, HIV/AIDS, allergies, and has even been connected to the pathophysiology of depression. Chronic inflammation can lead to and exacerbate cardiovascular disease, insulin resistance, and a host of other problems. It is also an important feature of obesity.
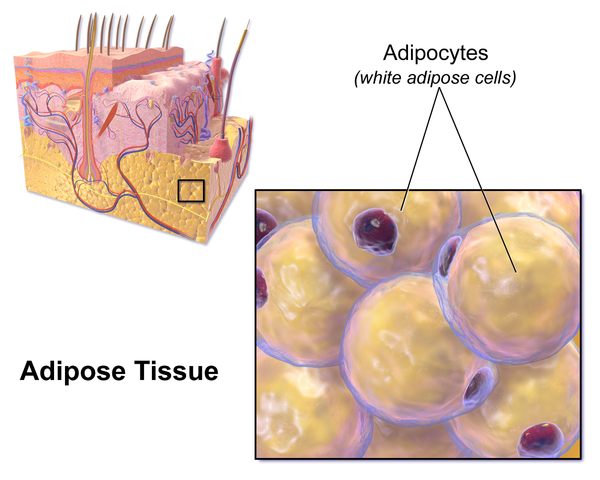
Our fat cells are more than just energy storage. They are a vital part of the endocrine system. We NEED our fat cells (adipocytes) to help regulate insulin sensitivity, for sex hormone production, to insure a functioning immune system, and regulate metabolism through hormones associated with the fat cells themselves (adiponectin and leptin are the most studied, resistin is another).
Adiponectin
Adiponectin is an important metabolism hormone, enhancing insulin sensitivity of skeletal muscle and the liver, helping clear glucose from the blood stream. Adiponectin decreases as body weight increases resulting in increased insulin resistance with weight gain. (1) There are genetic reasons for low adiponectin levels as well that are known to increase the risk of type 2 diabetes. (2)
Adiponectin affects inflammation in part with vascular disease. Adiponectin inhibits a cell signaling protein involved in inflammation called TNF-α and affects plaque formation in the arteries. It does this by inhibiting the conversion of immune cells called macrophages to foam cells which are implicated in plaque buildup in the arteries. (3)
Higher adiponectin levels are associated with lower body weight, better blood sugar control, and reduced inflammation, particularly in blood vessels.
Raising Adiponectin Levels
Your adiponectin levels are in part regulated by genetics but there are things you actually can do to raise adiponectin levels. Eating a diet high in fiber, getting plenty of omega-3s, exercise, and weight loss have all been shown to raise adiponectin levels. (4)
Leptin
Leptin is another hormone secreted by fat cells and is most known for suppressing hunger signals, but it has many other interesting effects as well. These include influences on the immune system, metabolism, bone and blood vessel formation, and reproduction.
Leptin levels directly correlate with the amount of energy stored in the adipose tissue. In obesity more leptin is secreted because there is more adipose tissue. Based on this you might expect heavier people to have less hunger, but we know this isn’t true. The reason obese people still have strong hunger signals is because there is a mechanism at play reducing the sensitivity of cells to leptin’s actions so its impacts on satiety are blunted.
High Leptin –> Elevated Immune Response –> Elevated Inflammation
The elevated level of circulating leptin in obesity contributes to low-grade chronic inflammation by upregulating inflammatory cytokines (like TNF, IL-12, and IL-6). Leptin levels also increase when there is other inflammatory stimulus, further increasing inflammation, (5) and has many other effects on both major immune system branches known as adaptive and innate immunity. Leptin’s influence on the immune response is also apparent when there are low levels, which leads to an impaired immune system—not producing an inflammatory response when you do want it. (6)
Elevated leptin levels and the associated elevation in inflammation are almost always associated with an elevated BMI.

What can we do to improve leptin sensitivity?
When weight is lost and leptin levels decline hunger signals increase. This is one of the reasons sustained weight loss is challenging, so finding ways to improve leptin sensitivity may improve outcomes of weight loss attempts.
- Improve triglyceride levels. Triglycerides are fats that are often associated with heart disease. They are a standard part of your cholesterol blood work. Having high triglycerides can induce leptin resistance. (7) Things that can help lower triglycerides include weight loss, exercise, a low carbohydrate diet, reducing alcohol consumption, and not smoking.
- Because leptin is associated with a feeling of fullness, doing other things to help you feel full like eating protein and healthy fats with each meal or snack can help create a more sustained blood sugar and curb hunger.
- Reduce total body inflammation because inflammation signals to the brain appear to be an important factor in leptin resistance. (8) I’ll discuss more on this later.
Resistin
Resistin is another adipose-derived hormone that appears to have a strong role in the pathogenesis of cardiovascular disease, type 2 diabetes, and inflammation. It is actually primarily secreted by macrophages but is also secreted by fat cells and is associated with the inflammation associated with fat. It promotes endothelial cell dysfunction (the cells lining blood vessels and lymphatic), increasing multiple pro-inflammatory mediators.
Reducing resistin
- Antioxidants – Studies have shown resistin can be reduced by consuming antioxidants like vitamin C, which you can get from your diet from eating fruits and vegetables.(9)
- Optimize Folate Levels – Folate has been shown to improve not only endothelial cell dysfunction, but also reduce homocysteine (which, when elevated is associated with atherosclerosis), as well as reduce resistin itself.(10)
- Olive oil may also be beneficial. Oleic acid, the primary fat in olive oil, was shown to reduce DNA expression of the resistin gene in fat cells.(11)
Macrophage Phenotypes
The following paragraphs get pretty science-y, so buckle up, or skip it.
A macrophage is an immune cell that I like to picture as Pac-Man, gobbling up inflammatory debris. For those of you paying attention, you may be saying, “Wait! Didn’t you say macrophages release resistin and can promote inflammation?!” Yes. They play a very interesting role in inflammation and obesity, being beneficial in some cases and inflammation-inducing in others.
I will explain (with the caveat that this is a bit of an over-simplification):
Macrophages come in 2 major types, M1 and M2 (with subsets of the M2 form), and they do different things. M1 is thought of as pro-inflammatory while M2 is associated with anti-inflammatory reactions. (12) Obesity pushes the balance to be M1-predominant resulting in more inflammation. (13)
What do you do to improve macrophage phenotype to M2?
More recently discovered compounds called resolvins, which are constituents of omega-3s, show promise as a potential therapy because they recruit macrophages. Not only that, resolvins and its precursor, DHA, actually promote the M2 phenotype which suppresses Th2 inflammation and fibrosis. (14) (15)
Researchers have indeed proposed that resolvins may be a potential treatment for obesity-associated inflammation but more research is necessary to determine the extent of its therapeutic application. In phase 2 clinical trials side effects have not been documented. Caution should be used however because macrophages do accumulate in obesity, especially with lymphatic impairment because a functioning lymphatic system is necessary to move these immune cells away from the periphery so they don’t accumulate and potentially cause damage. There may still be benefit due to the changes to an M2 phenotype as mentioned above, but it is still best if a healthcare provider determines if this may be an appropriate treatment on an individual basis.
Higher adiponectin can also promote M2 macrophages, so see above for ways to improve adiponectin levels.
How to Decrease Inflammation, and Lose Weight
Because so many chronic conditions are caused or exacerbated by inflammation, trying to decrease chronic inflammation is crucial.
Fat cells themselves aren’t the only source of inflammation in the body, so identifying other causes of inflammation and correcting this excessive immune response is important. One way to reduce inflammation associated with obesity probably goes without saying—lose weight and inflammation will likely decline. (16) Then how do you lose weight? We just learned how obesity promotes excess inflammation and excess inflammation promotes obesity, and this cycle is where many people get stuck. With so much contradictory information out there it can be hard to know where to start. There are things you can do to break out of this vicious cycle to both reduce inflammation AND lose weight! Start with the following steps:
- Eliminate or greatly reduce added sugar – Sugar is ubiquitous in the standard American diet. Some obvious like soda, baked goods, and candy, but some less obvious like added sugars in yogurt, pasta, crackers, and sauces. For many cutting sugar can be incredibly challenging. I find eliminating all added sugars for 14 days is highly effective at reducing or eliminating sugar cravings in many people. For others it is better to identify personal obstacles and individualize a plan to decrease sugar consumption. The American Heart Association and the American Diabetes Association recommend limiting added sugars to below 25 grams daily
- Address allergies – This includes identifying food allergies and sensitivities and removing them from the diet either through an elimination/re-challenge diet or testing, as well as addressing environmental allergies.
- Eat plants – Plants contain many different compounds such as polyphenols that help reduce oxidative damage in the body. Eating a rainbow of colors can help you get many different types of these phytonutrients.
- Other dietary strategies – Choose a diet that is right for you that also has anti-inflammatory benefits. The Mediterranean diet is generally a good dietary strategy for most people and has been shown to have numerous benefits on cardiovascular risk markers such as inflammation. It has even been shown to change the way DNA is expressed of several inflammation-related genes. (17) It is characterized by healthy fats like those from olive oil, nuts and seeds, poultry, eggs, seafood, whole grains, and lots of colorful fruits and vegetables. Some people may benefit from other diets such as the ketogenic/high fat low carb diet or certain dietary strategies such as intermittent fasting (limited eating window) for example. Consult your healthcare provider to help determine the diet that is right for you
- Stress reduction – The “stress hormone” cortisol causes increased inflammation after acute stressors, whether it be a vicious animal chasing you or sitting in traffic. It does this to get your body’s immune system prepared to repair or defend. In modern society we tend to have many low-grade stressors (i.e. getting the kids to the bus stop on time, that presentation you have to give, paying bills, etc) resulting in a lot of signals to increase inflammation. Meditation, breathing techniques, and even intermittent fasting can improve your response to stress.
- Optimize Sleep – Your sleep is very important for proper immune system function and getting poor sleep, especially over a long period of time is another chronic stressor. Also included would be addressing sleep apnea, a condition where the person’s breathing is interrupted many times throughout the night.
- Supplements – Supplements should be individualized to each person to maximize the benefit. There are multiple botanicals that appear to have anti-inflammatory effects, in some cases supplementation of high quality omega-3 fatty acids is beneficial, and the previously mentioned resolvins also have potential. Since sources of inflammation can vary greatly I recommend seeing a provider, such as a naturopathic physician, who is well-informed about supplement quality, herb-nutrient-drug interactions, and evidence-based use of these formulas.
Support the Lymphatic and Vascular Systems
The lymphatic system is an immune network and waste removal system. When inflammation is present we need our lymphatic system to clear inflammatory debris. In conditions like lymphedema or late stage lipedema with lymphatic involvement, this system isn’t working properly and fluid builds up in tissues, including inflammatory proteins and immune cells like macrophages.
- Again, eat plenty of phytonutrients – Phytonutrients have a vast array of beneficial actions on the body. Proanthocyanidins are primarily found in berries. These and other compounds can help rebalance connective tissue turnover in venous walls (i.e. matrix metalloproteinases vs. tissue-building enzymes), help reduce inflammation, and even positively affect DNA expression. Proanthocyanidins and tannins have been shown to be beneficial in chronic venous insufficiency and lymphatic insufficiency.(18)
- Skin Brushing – Skin brushing or dry brushing is a technique that reportedly helps aid lymphatic flow. It is done by using a dry, natural fiber brush and gently brushing your body surface in the direction of lymphatic flow.
- Exercise – Both the increase in blood flow and the muscle contractions helping pump lymphatics are two of the many benefits exercise can provide for the lymphatic system. Whether it’s walking, swimming, or jumping on a trampoline, being active is vital for vascular and lymphatic health.
- Other lymphatic and vascular support options like medications and supplements should be personalized to you to address things like cardiovascular disease or lymphedema for example.
This article is intended only to inform, not to diagnose or treat. Please see your healthcare provider for evaluation of any health concerns.
If you are looking for a doctor who specializes in treating these issues, Dr. Aylah Clark will personalize the process for your individual needs. To schedule an appointment with Dr. Clark, please call 860-661-4662 and Liz our office manager will happily get you set up!
Works Cited
- Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Arita, Y, Khara, S and Ouchi, N. s.l. : Biochem Biophys Res Commun, 1999, Vol. 257, pp. 79-83.
- Association of adiponectin mutation with type 2 diabetes: a candidate gene for the insulin resistasnce syndrome diabetes. Kondo, H, Shimomura, I and Matsukawa, Y. s.l. : Google Scholar, 2002, Vol. 51, pp. 2325-8.
- Adipocyte-derived plasma protein, adiponectin, suppreses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Ouchi, N, Kihara, S and Arita, Y. s.l. : Circulation, 2001, Vol. 103, pp. 1507-63.
- Effect of diet on adiponectin levels in blood. Silva, FM, de Almeida, JC and Feoli, AM. 10, s.l. : Nutr Rev, 2011, Vol. 69, pp. 599-612.
- Leptin enhances TNF-α production via p38 and JNK MAPK in LPS-stimulated Kupffer cells. Shen, J, et al., et al. s.l. : Life Sci, 2005, Vol. 77, pp. 1502-15.
- Leptin and Inflammation. Iikuni, Noriko, et al., et al. 2, s.l. : Curr Immunol Rev, 2008, Vol. 4, pp. 70-79.
- Triglycerides induce leptin resistance at the blood-brain barrier. Banks, WA, et al., et al. 5, s.l. : Diabetes, 2004, Vol. 53, pp. 1253-60.
- Regulation of food intake, energy balance, and body fat mass: implications for the pathogenesis and treatment of obesity. Guyenet, Stephan J and Schwartz, Michael W. 3, s.l. : J Clin Endocrinol Metab, 2012, Vol. 97, pp. 745-755.
- Efficacy of antioxidant treatement in reducing resistin serum levels: a randomized study. Bo, Simona and Ciccone, Giovannino. 5, s.l. : PLoS Clin Trials, 2007, Vol. 2, p. e17.
- Folic acid consumption reduces resistin level and restores blunted acetylcholine-induced aortic relaxation in obese/diabetic mice. SEto, SW, et al., et al. 9, s.l. : J Nutr Biochem, 2010, Vol. 21, pp. 872-80.
- Effects of metformin and oleic acid on adipocyte expression of resistin. Rea, R and Donnelley, R. 1, s.l. : Diabetes Obes Metab, 2006, Vol. 8, pp. 105-9.
- Macrophage polarization in inflammatory disease. Liu, YC, et al., et al. 5, s.l. : Int J Biol Sci, 2014, Vol. 10, pp. 520-529.
- Obesity induces a phenotypic switch in adipose tissue macrophage polarization. Lumeng, CN, Bodzin, JL and Saltiel, AR. 2007, J Clin Invest, Vol. 117, pp. 175-84.
- Resolvin D1 and Its Precursor Docosahexaenoic Acid Promote Resolutino of Adipose Tissue Inflammation by Eliciting Macrophage Polarization toward an M2-Like Phenotype. Titos, Esther, et al., et al. s.l. : J Immunol, October 17, 2011.
- Resolvin D1 Polarizes Primary Human Macrophages toward a Proresolution Phenotype through GPR32. Schmid, Mattia, et al., et al. 8, s.l. : J Immunol, 2016, Vol. 196, pp. 3429-3437.
- Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Nicklas, BJ, et al., et al. 4, s.l. : Am J Clin Nutr, 2004, Vol. 79, pp. 544-51.
- Adherence to Mediterranean diet is associated with methylation changes in inflammatino-related genes in peripheral blood cells. Arpón, A, et al., et al. s.l. : J Physiol Biochem, 2017.
- Microcirculatory changes in patients with chroni venous and lymphatic insuficiency and heavy leg symptoms before and after therapy with procyanidol oligomers (laser-Doppler study). Daróczy, J, Pál, A and Blaskó, G. 22, s.l. : Orv Hetil, 2004, Vol. 145, pp. 1177-81.
[/fusion_builder_column][/fusion_builder_row][/fusion_builder_container]





Leave A Comment