Dr. Aylah Clark
Lipedema is an adipose tissue (fat tissue) disorder primarily affecting the lower extremities and sometimes arms that spares the hands and feet. It almost exclusively affects women with symptoms beginning often after hormonal change like puberty, menopause, or pregnancy.

There is a lot we don’t know about lipedema. We don’t know exactly why it happens or what sets it off. It is thought to have a genetic component as it is common for people with lipedema to have family members with it (or suspected to have it). It is also thought that estrogen, or changes in estrogen levels, may play a role in triggering the condition since it almost never happens in men and the men it does happen to tend to have conditions that have caused higher estrogen. Because of its correlation with hormonal change, some think it may be set off by changes to genetic expression. While DNA itself doesn’t change, external factors, such as hormones, can change the way it is read. (The study of how external factors can modify gene expression is called epigenetics.)
In lipedema, some of the physical effects on the body include a nodular texture to the affected fat tissue that is often painful to the touch, a columnar appearance of the legs that can create a cuffing appearance at the wrists or ankles, and outpouchings of fat tissue especially around the knees which can interfere with mobility.
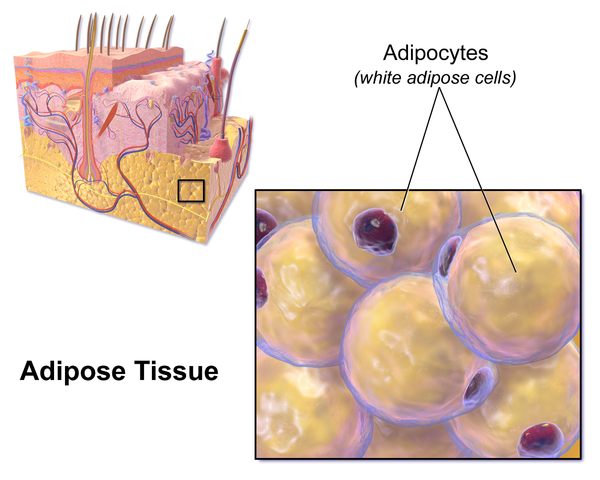
Less apparent is what happens microscopically. Fat cells grow in both size and number. This causes them to become low on oxygen (hypoxic). When cells don’t have enough oxygen, they become damaged, have altered metabolism including mitochondrial impairment, and they can die. As cells die, your immune system sends in immune cells that act like Pacman, helping to clear the debris. Inflammation is necessary to heal, but it also can result in further damage when it can’t finish the job and goes on for too long, resulting in harmful chronic inflammation.
Inflammation causes a cascade of other problems. Tissue becomes fibrotic and thickened, including the cell walls of fat cells and the walls of blood vessels. This process is called microangiopathy when it happens to blood vessels. These blood vessels become more fragile and leakier as there is increased pressure from incoming fluid (immune response, blood flow, etc.). Low oxygen levels also signal more small blood vessels (microvasculature) to be formed to bring more oxygen to the area. Ultimately this appears to cause an overwhelming of the lymphatic pumps due to increased flow into the area without the increase in flow out of the area (i.e. more blood vessels and fluid in without an increase lymphatic and venous channels out). Many patients with lipedema also develop lymphedema (lymphedema is when lymphatic fluid, which is important for immune function, builds up due to impaired function or blockage of lymphatic vessels).
As we learn more about what is happening in lipedema we can find more targets for treatment. Relatively few people are familiar with lipedema even in the medical community and more research is needed to fully understand the condition and which treatments are effective.
Naturopathically there are many ways we can help address underlying drivers of the condition by reducing inflammation, reducing macrophage infiltration into fat cells, helping restore metabolism of fat cells, supporting the integrity of the vasculature, improving hormone balance, reducing oxidative damage to tissue, and improving quality of life by supporting the whole person. I will be discussing some of these potential treatments that help these systems work together again in more detail in upcoming articles.
For more background information about lipedema click here or for information on how inflammation affects body weight click here. If you want to find out which treatments will most help your specific situation, schedule an appointment with Dr. Clark today!




Leave A Comment