Celiac disease is an autoimmune disease where gluten consumption triggers an inflammatory response and damage to the intestines. It is caused by a complex interaction between genetic predisposition, intestinal microbiome, environment, and the immune system.
Symptoms & Diagnosis
Symptoms
can vary widely but can include gastrointestinal symptoms such as abdominal
pain, diarrhea, bloating, and mouth sores, but can also lead to weight loss or
failure to thrive, fatigue, dermatitis herpetiformis (a skin condition),
neurological symptoms, hormone disruption such as irregular periods,
infertility, early menopause, and nutrient deficiencies leading to
osteopenia/osteoporosis (bone loss).
Diagnosis is usually done by blood test but is confirmed by intestinal biopsy. The primary treatment is a gluten-free diet and occasionally corticosteroids. Because nutrient deficiencies are a concern it may be appropriate to do labs to evaluate levels of iron, folate, vitamin B12, carotene, albumin, prothrombin time, and calcium levels.
However, some people with celiac disease continue to experience symptoms (gastrointestinal or otherwise) despite the elimination of gluten from the diet. Here are 6 of the most common reasons that I see people with celiac disease continue to have symptoms:
1 – You’re still getting exposed to gluten
Since eliminating major sources of gluten you probably noticed major improvements in how you feel, but often people are still getting exposed to gluten at some level. This is either because they are unaware of lesser known sources of gluten, they aren’t as careful as they think, other people are preparing foods that are uninformed about gluten and celiac disease (like in restaurants), or there is contamination.
Contamination

Contamination can happen when foods that are naturally gluten-free are prepared in the same area as gluten-containing foods, or they are manufactured in a facility that doesn’t adequately clean the machinery between processing gluten-containing and gluten-free foods. Oats are a good example of more highly contaminated gluten-free foods and is the reason why you can buy gluten-free oats, even though they are inherently gluten-free.
Hidden Sources
If you have celiac disease you are probably well aware that gluten is in foods like bread, pasta, cereals, beer, and so on, but there are many other not-so-obvious sources as well. For example, French fries, soy sauce, salad dressing, marinades, processed meat, vegetarian meat substitutes, soup, gravy, cheesecake filling, and even in omelets or other egg dishes at restaurants (they sometimes add pancake batter) can all have gluten. Additionally, with the increased use of paper straws it is important to know that many of these straws contain gluten. Opt out of straws or bring your own glass/stainless steel straw.
Reading Labels
It is important to read labels because some things you may think must be gluten-free, like corn flakes for example, are prepared with something like malt extract that contains gluten. Words to look out for on packaging that can indicate gluten is present include malt, brewer’s yeast, and starch to name a few.
Eating Out

It’s also important to tell restaurants you have a gluten allergy, because even if the dish appears to be inherently gluten-free, there could be ingredients like sauces that have gluten. Sometimes restaurants aren’t as good at avoiding contamination or educating staff about what may contain gluten, so eating at restaurants that are informed is important. Look for a local gluten-free guide (like www.wickedglutenfree.com) to help you find safe places to eat.
2 – Your intestines have not yet healed
In celiac disease the damage to the intestines is known as villous atrophy and this is the primary cause for symptoms. Once gluten is eliminated from the diet the body is able to repair itself. This can take time however and varies by person and whether gluten has been completely eliminated or not. Some sources say this could take anywhere from weeks to years, while some never completely heal.
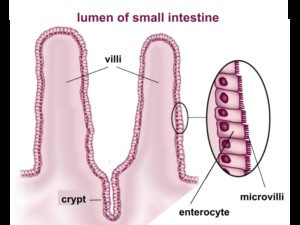
Usually repair begins quickly– within a week of being gluten-free and some people notice changes in that time frame, while others may not notice a difference at all at this point. Patients typically have a noticeable improvement in symptoms in 2-3 months, and the majority heal completely within 3-6 months but this can vary widely depending on the severity of the disease and other factors.
3 – You’re not digesting optimally
It is common for people with celiac disease (especially early in diagnosis) to have lactose intolerance or intolerance to other foods because they are not digesting foods as well. This is because you aren’t producing sufficient enzymes (like lactase to break down lactose). Lactase cleaves lactose into two different sugars your body can absorb known as galactose and glucose. Your body produces these enzymes in the intestines, and because there is intestinal damage in celiac disease, these enzymes are not produced at optimal levels.
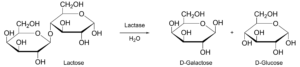
Other enzymes that may be sub-optimal include peptidases that cleave amino acids off of peptides (essentially small proteins), lipases that help you break down fats, and other enzymes that help you in the final stages of breaking down starches/carbohydrates (sucrose-isomaltase and maltase-glucoamylase).
As your intestines heal your ability to digest and produce these enzymes should improve and you may no longer have lactose intolerance.
4 – Microscopic colitis
Microscopic colitis is an inflammatory condition of the colon with a lot of symptom overlap with celiac disease – cramping, abdominal pain, and diarrhea. Microscopic colitis is also much more common in people with celiac disease than the general population—50 times higher! The most common demographic to have both celiac disease and microscopic colitis is middle-aged women. (1)
Microscopic colitis would need to be ruled out by your gastroenterologist by colonoscopy or flexible sigmoidoscopy with a biopsy.
5 – Relying too much on gluten-free substitutes

Sometimes when people go gluten-free they can heavily rely on pre-packaged foods that have “gluten-free” on the label, but aren’t necessarily healthy foods. They often contain lots of starch and other foods that can negatively impact your blood sugar and aren’t as beneficial for gut health as vegetables for example. Instead of turning to these heavily-processed foods, try eating more whole foods that are naturally gluten-free like fruits, vegetables, quinoa, rice, and proteins like fish, poultry, egg, grass-fed beef, etc.
6 – Bacterial Imbalance/Dysbiosis
Bacterial imbalance is known to occur in celiac disease, whether the person has been gluten-free or is recently diagnosed. This disrupted microbiome is a known contributor to persistent gastrointestinal symptoms in celiac disease and influences the way the disease manifests (i.e. with dermatitis herpetiformis, inflammation levels, etc). (2)
Then comes the chicken or the egg question. Is the dysbiosis caused by celiac disease or does the abnormal bacteria trigger the disease? As it turns out, a little of both. The bacterial imbalance is in part influenced by your DNA. Certain genes and/or changes in their expression common in celiac disease can actually change what bacteria end up colonizing your gut. Besides your DNA, other things can lead to dysbiosis like antibiotics, steroids, and the food you eat.
The bacteria also influence the environment that may trigger the abnormal response to gluten. In autoimmune diseases there is a problem with the body’s immune system tolerating part of itself. Part of this loss of tolerance is thought to come from the body’s immune response to commensal (good) bacteria vs. inflammation-promoting/problematic bacteria. There are also specific interactions between bacterial species and immune system responses such as immune cell activity which can result in increased inflammation.
Treating Dysbiosis
Modulating intestinal bacteria could potentially reduce risk of celiac disease in high risk individuals or decrease symptoms in those with persistent symptoms after gluten elimination.
What are the specific changes that happen to the microbiome and what can be done about it?
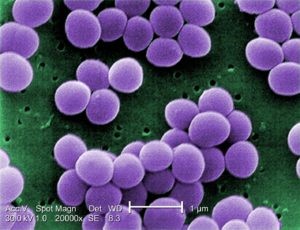
Probiotics are an obvious consideration, but treatment should be individualized to address the specific imbalance that occurs in celiac disease and when possible, specific to each person’s microbiome. This is an emerging field but there are promising studies. Research indicates that this imbalance in celiac disease typically results in reduced Bifidobacterium spp. and B. longum with increased levels of Bacteroidetes. High levels of enterobacteria and staphylococci that are seen in untreated celiac disease appears to resolve with a gluten-free diet. (3) (4) Studies with probiotic treatment has been positive with a reduction in some but not all symptoms using B. infantis, (5) reduced Bacteroidetes and improved levels of inflammatory markers with B. longum, (6) and reduced inflammatory markers in children with B. breve. (7)
If you have celiac disease but are still experiencing symptoms, see your healthcare provider to determine the best course of treatment.
This article is intended only to inform, not to diagnose or treat. Please see your healthcare provider for evaluation of any health concerns.
If you are looking for a doctor who specializes in treating these issues, Dr. Aylah Clark will personalize the process for your individual needs. To schedule an appointment with Dr. Clark, please call 860-661-4662 and Liz our office manager will happily get you set up!
Resources:
- www.wickedglutenfree.com
- www.celiac.org
- Everything You Ever Wanted to Know About Gluten & Beer and Your Go-To List for Gluten-Free Beers
- To learn more about the importance of probiotic quality and individualizing treatment go here.
Works Cited
- Systematic review: microscopic colitis. Nyhlin, N, Bohr, J and Eriksson, S. s.l. : Aliment Pharmacol Ther, 2006, Vol. 23, pp. 1525-34.
- Intestinal Microbiota and Celiac Disease: Cause, Consequence, or Co-Evolution? Cenit, María Carmen, et al. 8, s.l. : Nutrients, 2015, Vol. 7, pp. 6900-6923.
- Specific duodenal and faecal baterial groups associated with pediatric coeliac disease. Collado, M.C., et al. s.l. : J Clin Pathol, 2009, Vol. 62, pp. 264-269.
- Imbalances in faecal and duodenal bifidobacterium species composition in active and non-active coeliac disease. Collado, M.C., et al. s.l. : BMC Microbiol, 2008, Vol. 8, p. 232.
- Exploratory, randomized, double-blind, placebo-controlled study on the effects of bifidobacterium infantis natren life start strain super strain in active celiac disease. Smecuol, E, et al. s.l. : J Clin Gastroenterol, 2013, Vol. 47, pp. 139-147.
- Double-blind, randomised, placebo-controlled intervention trial to evaluate the effects of bifidobacterium longum cect 7347 in children with newly diagnosed coeliac disease. Olivares, M, et al. s.l. : Br J Nutr, 2014, Vol. 112, pp. 30-40.
- Administration of Bifidobacterium breve decreases the production of TNF-alpha in children with celiac disease. Klemenak, M, et al. s.l. : Dig Dis Sci, 2015.




Leave A Comment